This article was first published by the Innovative Genomics Institute.
2020 was a big year for CRISPR — the discoveries of new Cas proteins, use of CRISPR technology to study and develop diagnostic tests of COVID-19, a Nobel Prize, and more. The past year has also brought results from clinical trials using CRISPR technology, which we first reported on in 2019, and the start of new clinical trials.
In this article, we will go over the basics of clinical trials and then map out the current CRISPR-based trials from disease background to what we really hope to learn from these trials.
CLINICAL TRIAL BASICS
In the United States, the Food and Drug Administration (FDA) evaluates new disease treatments for safety and efficacy through clinical trials on patient volunteers. Early trials look at safety and side effects. Later trials test efficacy and compare new therapies with standard treatments.
The current trials using CRISPR-based treatments are still in early stages. That means that even if the treatments are safe and effective, they’re likely still a few years away from FDA approval and being broadly available to patients.
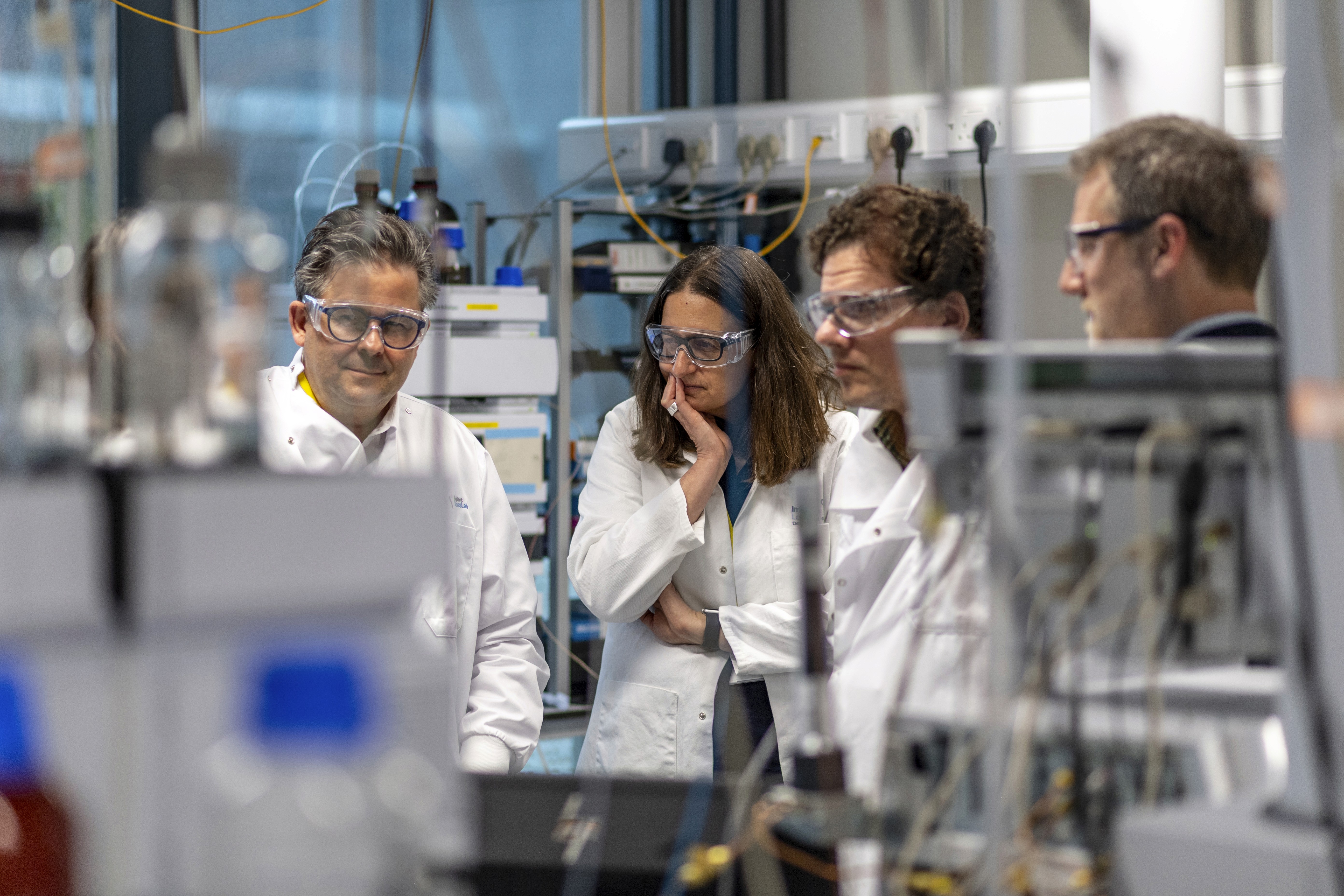
The advent of CRISPR technology opens up new possibilities in precision medicine. Current trials are underway in five treatment areas: blood disorders, cancers, eye disease, chronic infections, and protein-folding disorders. All current CRISPR clinical trials are intended to edit specific cells or tissues without affecting sperm or eggs, meaning no DNA changes can be passed onto future generations.
BLOOD DISORDERS
DISEASE BACKGROUNDS
Red blood cells use hemoglobin to carry oxygen from the lungs to all the tissues of the body. Mutations in a gene that encodes part of the hemoglobin molecule cause two different genetic disorders: sickle cell disease (SCD) and beta thalassemia.
In sickle cell disease (SCD), red blood cells are misshapen. Their crescent or “sickle” shape makes them block blood vessels, slowing or stopping blood flow. This causes sudden, severe pain. Complications include chronic pain, organ damage, strokes, and anemia. In beta thalassemia, patients do not make enough hemoglobin. This leads to anemia and fatigue. In more severe cases, patients have organ damage, especially to the liver, bones, and heart. Both diseases can be fatal.
There are some treatments available, but often, patients still suffer severe symptoms and complications from their diseases. Patients with more severe SCD and beta thalassemia need frequent blood transfusions. Bone marrow transplant can be curative; however, this can only be done when a healthy, matching donor can be found. This is not an option for most SCD or beta thalassemia patients.
TREATMENT STRATEGIES
The approach taken to treat blood disorders with CRISPR technology doesn’t directly fix the gene variants that cause disease, but uses a clever workaround: instead of directly fixing the disease-causing mutations, the goal is to increase levels of fetal hemoglobin. This is a form of hemoglobin that fetuses make in the womb, but children and adults don’t make. It is not entirely understood why humans switch from one form of hemoglobin to the other, but fetal hemoglobin can take the place of defective adult hemoglobin in red blood cells. This treatment can be used to treat both beta thalassemia and SCD.