Longevity
The Prevention Economy Has Arrived. Is Your Clinic Ready?
A $150 Million Signal That Changes Everything
Curative just raised $150 million in Series B funding. If you're running a preventive medicine or longevity clinic, this should matter to you more than any longevity biotech announcement you've read this year.
Not because Curative is a direct competitor. They're not. They're a health insurance company building employer-based plans around a radical premise: eliminate all out-of-pocket costs (no copays, no deductibles, no coinsurance) if members complete an annual preventive "Baseline Visit."
The model works. Curative reports measurable outcomes within the first year of enrollment: 20% increase in primary care engagement, 30% fewer hospitalizations, and up to 40% lower drug costs.
Let that sink in. A payer just raised $150 million to bet that prevention-first healthcare is not just better for patients, but better for business.
This is the signal that the prevention economy has moved from theory to operational reality. And it creates both enormous opportunity and serious operational challenges for the clinics positioned to deliver this care.
Why This Matters Now
For years, we've heard that healthcare needs to shift from sick care to prevention. The logic was obvious. The incentives were broken.
Fee-for-service medicine rewarded volume, not outcomes. Insurers made money by denying claims and managing risk pools, not by keeping people healthy. Patients only engaged with healthcare when something went wrong.
The result? A system optimized for expensive interventions on established disease rather than low-cost prevention of dysfunction.
But something changed. Employers are now the largest healthcare purchasers in the US, and they're tired of watching premiums climb while employee health declines. They're looking for models that reduce long-term costs, improve productivity, and demonstrate measurable outcomes.
Payers like Curative are responding by building prevention-first infrastructure. They're not asking "how do we pay for sick care more efficiently?" They're asking "how do we keep people from getting sick in the first place?"
This creates a market for preventive medicine clinics that didn't exist five years ago. Employers want to buy what you're selling. Payers are building reimbursement models around it. The demand is real, but demand isn't enough.
The Three Forces Converging Right Now
Three separate trends are colliding to create this moment, and understanding all three is critical to seeing where this goes.
1. Payer Models Are Shifting Upstream
Curative isn't alone. Value-based care models, accountable care organizations, and direct primary care arrangements are all variations on the same theme: align incentives around keeping people healthy rather than treating them when they're sick.
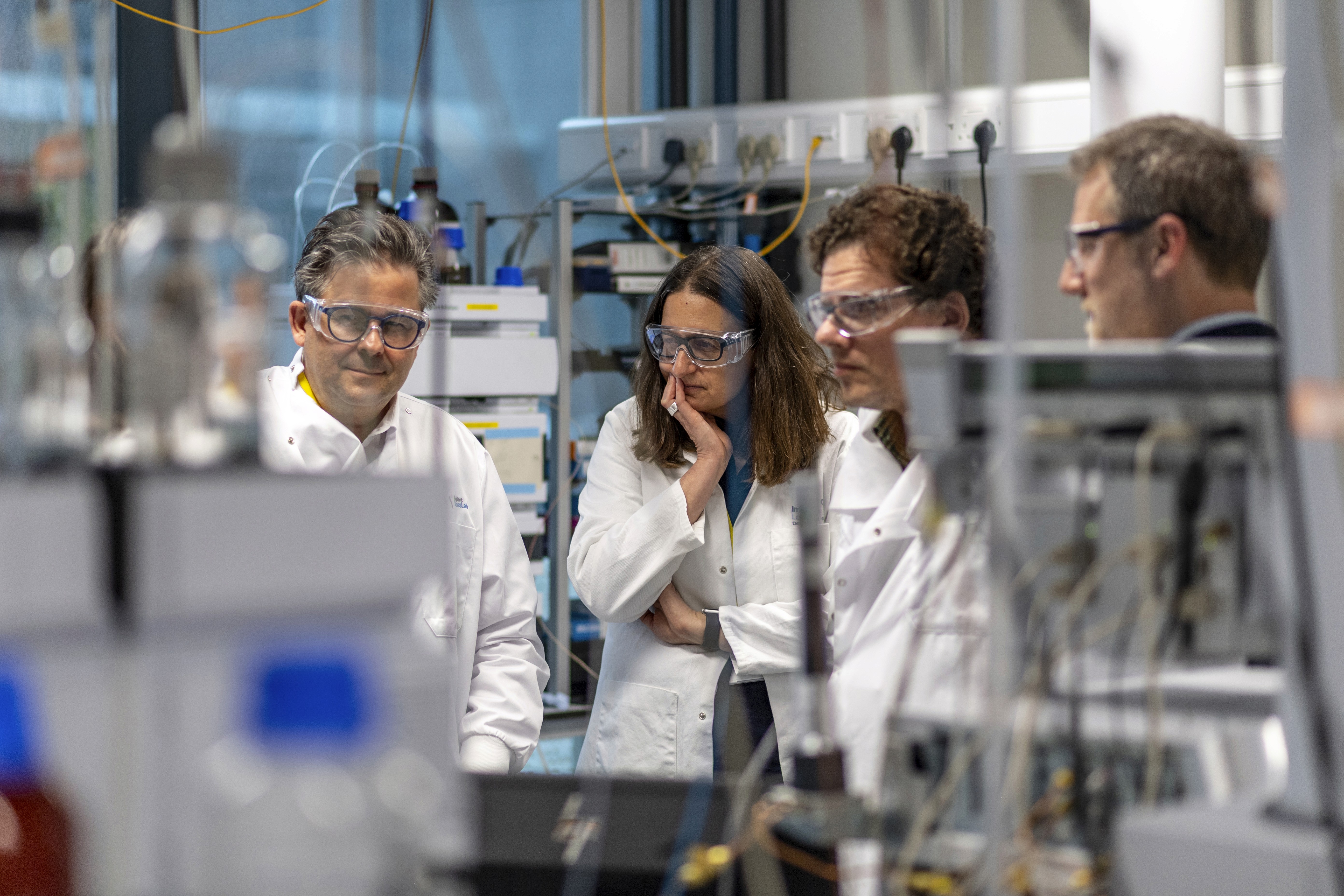
These models need clinical partners who can deliver preventive care at scale. Not just annual physicals with standard labs. Real prevention: comprehensive biomarker panels, lifestyle interventions, continuous monitoring, early detection of subclinical dysfunction.
This is exactly what functional medicine and longevity clinics do. The infrastructure payers are building needs you.
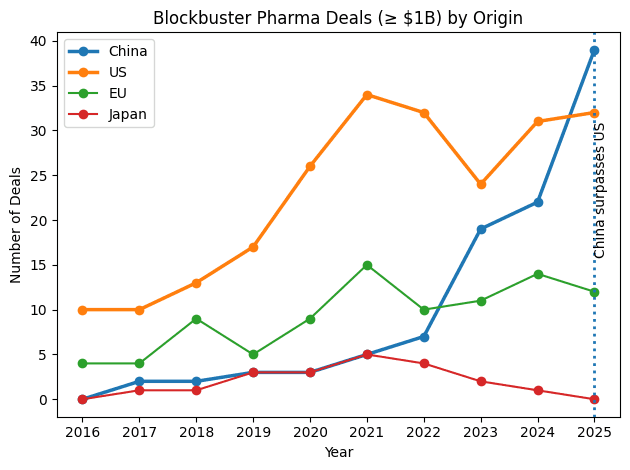
2. Science Is Accelerating
Longevity biotech is getting serious. Therapies targeting cellular senescence, metabolic health, mitochondrial function, and epigenetic aging are moving from research to clinical trials.
Companies developing these interventions need clinical networks to deliver them. They need practitioners who understand root-cause medicine, multi-system interventions, and outcome tracking. They need clinics with the data infrastructure to participate in trials, measure efficacy, and demonstrate real-world effectiveness.
Again, this is what you already do. The question is whether you have the operational systems to participate at scale.
3. The Infrastructure Gap Is Becoming Obvious
Here's where it gets interesting.
Payers want to buy prevention. Science is delivering better interventions. Patients want personalized, proactive care.
But most preventive medicine clinics operate on fragmented infrastructure:
Patient data scattered across EHRs, lab portals, wearable apps, and paper forms
No unified view of longitudinal health trajectories
Manual tracking of adherence and outcomes
Limited ability to demonstrate ROI to employers or payers
No standardized reporting for population health metrics
You can deliver excellent care to individual patients. But can you prove outcomes at the population level? Can you generate the data payers need to justify reimbursement? Can you scale your model without drowning in administrative overhead?
This is the gap. And it's the reason most preventive medicine clinics can't participate in the prevention economy even though the demand exists.
What Clinically Governed Infrastructure Actually Means
The solution isn't just "better software." It's a fundamentally different approach to how preventive care gets operationalized.
Unified Patient Data Layer
Every patient generates health data from multiple sources: clinic visits, lab results, genetic testing, wearable devices, patient-reported outcomes. In most practices, this data lives in silos.
A unified data layer brings it together. Not just storing it in one place, but integrating it into a coherent longitudinal record that shows trajectories, identifies patterns, and enables prediction.
This is the foundation. Without it, you're practicing reactive medicine with preventive intentions.
Personalized Protocol Engine
Generic wellness plans don't work. Prevention requires personalization based on individual biomarkers, genetic profiles, lifestyle factors, and health goals.
But personalization at scale requires systems. You need protocols that adapt based on patient data, track adherence, flag when interventions aren't working, and provide clinical decision support without creating overwhelming cognitive load.
The goal isn't to replace clinical judgment. It's to amplify it by handling the complexity that exceeds human cognitive bandwidth.
Outcome Tracking and Reporting
This is where most preventive medicine practices fail operationally. You know your interventions work. You see patients improve. But can you demonstrate it systematically?
Payers and employers want data:
What percentage of patients improve their metabolic markers?
How many avoid progression to chronic disease?
What's the average change in biological age?
Which interventions drive the best outcomes for which patient phenotypes?
If you can't answer these questions with data, you can't participate in value-based contracts. You can't demonstrate ROI to employers. You can't contribute to the evidence base that legitimizes preventive medicine.
Clinical Governance
Here's what separates infrastructure from automation. Clinical governance means physicians remain the decision-makers.
AI can identify patterns. Algorithms can flag concerning trends. Systems can suggest interventions. But the clinical validation, protocol approval, and treatment decisions remain under physician oversight.
This isn't just about quality. It's about trust. Payers, employers, and patients need confidence that preventive care is rigorous, evidence-based, and clinically supervised. Black box algorithms don't build that trust. Physician-governed platforms do.
The Operational Reality for Clinics
Let's get practical about what this means for a preventive medicine clinic trying to scale.
Scenario: A Functional Medicine Practice
You run a successful functional medicine practice. You see 20-30 patients per week. You order comprehensive labs, track biomarkers over time, create personalized protocols, and get great outcomes.
A local employer reaches out. They want to offer your services to their 500 employees as a preventive health benefit. They'll pay a per-employee-per-month fee. They want quarterly outcome reports showing engagement rates, health improvements, and ROI.
Can you do it?
With your current systems?
How will you track 500 patient trajectories across multiple biomarkers?
How will you generate personalized protocols for hundreds of people?
How will you monitor adherence and flag who needs clinical outreach?
How will you aggregate outcomes data for reporting?
How will you handle the administrative load without hiring a small army?
Without proper infrastructure, this opportunity becomes an operational nightmare. You either turn it down (leaving money and impact on the table) or accept it and drown in manual work that pulls you away from clinical practice.
This is the infrastructure gap in practice.
What We Built at Longevitix (And Why)
We built Longevitix because we saw this gap from the clinical side. Preventive medicine works. The science is solid. The patient outcomes are real. But the operational systems to deliver it at scale didn't exist. So we built them:
Clinical Clarity Engine: Unifies patient data from labs, wearables, genetics, and patient inputs into longitudinal trajectories. Identifies patterns across multi-modal data streams. Surfaces what matters while filtering noise.
Multi-Layer Clinical Safeguard (MLCS)™: Ensures AI-driven insights remain under physician oversight. Clinical validation gates, bias detection, real-time guardrails, and continuous monitoring. Technology amplifies clinical judgment without replacing it.
Protocol Automation: Personalized prevention plans that adapt based on patient data. Track adherence, flag non-responders, provide clinical decision support. Scale personalization without scaling workload.
Outcome Analytics: Aggregate population health metrics. Track intervention effectiveness. Generate reports for payers, employers, and quality improvement. Turn individual patient care into demonstrable population outcomes.
This isn't just practice management software. It's the operational infrastructure that lets preventive medicine clinics participate in the prevention economy being built by payers like Curative and funded by longevity biotech.
The Window Is Open (But Not Forever)
Here's the uncomfortable truth. The prevention economy is happening with or without the current generation of preventive medicine practitioners.
If functional medicine clinics, integrative practices, and longevity doctors don't build the operational systems to deliver at scale, someone else will. Large health systems will create "wellness divisions." Tech companies will build direct-to-consumer platforms. Payers will contract with whoever can demonstrate outcomes and handle population health management.
The clinical expertise you have is valuable. The patient relationships you've built matter. The outcomes you generate are real.
But expertise without infrastructure doesn't scale. And in a market where payers are investing hundreds of millions in prevention-first models, scale matters.
The good news? You have a head start. You've been doing this work for years while conventional medicine ignored it. You understand root-cause interventions, multi-system thinking, and personalized protocols. You know how to track biomarkers and interpret trajectories.
You just need the operational systems to do it at the scale the market is demanding.
Three Questions Every Preventive Medicine Clinic Should Ask
1. Can you demonstrate outcomes at the population level?
Individual patient success stories are powerful. But payers and employers need aggregate data. If you can't show that 60% of your patients improve metabolic markers within six months, or that your interventions reduce disease progression by measurable amounts, you can't compete for value-based contracts.
2. Can you handle 10x patient volume without 10x administrative staff?
Scale requires systems. If doubling your patient load means doubling your team, your model doesn't scale. Look for infrastructure that automates data integration, protocol generation, adherence tracking, and outcome reporting.
3. Is your platform ready for regulatory and payer scrutiny?
When you contract with employers or payers, you'll face compliance requirements, data security standards, and outcome verification processes. Your infrastructure needs to meet those standards today, not when you land the first contract.
Being Right Doesn't Mean You'll Win
The irony is striking: Preventive medicine practitioners have been right for decades about how healthcare should work. You've been treating root causes while everyone else managed symptoms. You've been tracking trajectories while others looked at snapshots. You've been preventing disease while the system waited for it to arrive. And now the market is finally catching up.
But being right doesn't guarantee you'll benefit from being right. The prevention economy will get built regardless. The question is who builds it.
Will it be the practitioners who pioneered this approach but lack the operational systems to scale? Or will it be well-capitalized newcomers who understand infrastructure but lack your clinical depth? Well, it’s probably the latter, unless the former builds different systems fast.
You can't win a data-driven market with paper-based operations. You can't participate in value-based contracts without value-based measurement. You can't scale personalized medicine with manual processes.
The clinical innovation happened in your clinics. The operational innovation needs to happen there too. That's the real race. Not against other preventive medicine practices. Against the clock.