Engineered Human Therapies
Can Synthetic Biology Aid in The Race Against Rare Infectious Diseases?
Synthetic biology approaches are advancing vaccines and therapeutics for otherwise neglected rare infectious diseases
AI Image Created Using DALL-E
Over the last two decades, India and Bangladesh have witnessed frequent outbreaks of Nipah—a viral infection that can cause severe encephalitis and death—including one as recently as September 2023. In the same period, monkeypox, another rare viral infection, appeared in the US, Nigeria, and Europe.

While these outbreaks were contained, there are still no approved therapeutics for either disease. Nipah and monkeypox are two of the many rare infectious diseases. Likewise, most lack any vaccines or therapeutics.
Infectious diseases are more common in tropical regions owing to the greater biodiversity of pathogens, vectors, and hosts. And since the tropics are also home to a large number of low-income countries, many tropical infections, particularly rarer ones, remain neglected. Moreover, rare disease patients are also underserved for a range of reasons, including lack of data and commercial incentives. While most rare diseases are genetic, a minority are rare infections.
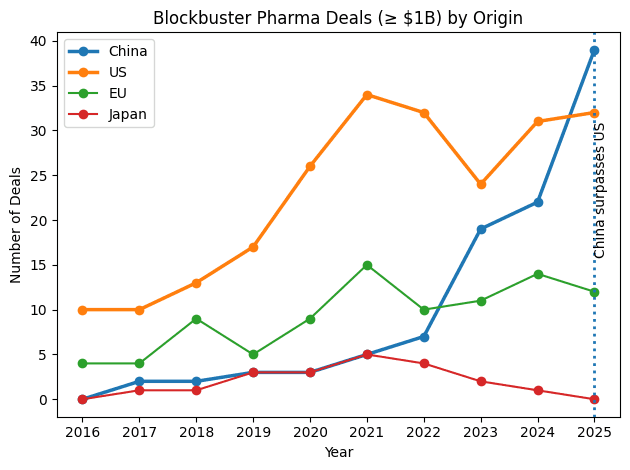
While rare genetic diseases have seen some attention in recent years, rare infections exist at the intersection of the two unmet needs and usually receive little attention. However, today's rare infectious disease could be tomorrow's global pandemic. Due to this growing awakening and new synthetic biology approaches, companies are beginning to focus on rare infections.
Effective Vaccines Serve Unmet Needs
Like with all infectious diseases, vaccines are the most potent weapon in the fight against rare infections. In fact, some infectious diseases, such as polio, are rare today solely because vaccines exist for them. Among those rare infections that lack vaccines, some have existed at stable prevalences, whereas others are emerging threats that could become more prevalent.
However, developing vaccines or therapeutic interventions for infectious diseases, particularly rare ones, is challenging. “It is not always clear who is at risk, who gets exposed, who dies, and what's different between those who get sick or die and who don't,” said Stephen Thomas, an infectious disease researcher at SUNY Upstate Medical University.

Thomas said that platform technologies are crucial to tackling existing and emerging infectious diseases. A platform technology is a mechanism or delivery method that can be adapted to multiple vaccines. This enhances the speed of vaccine development and allows companies to diversify and derisk their portfolios. Emphasizing their importance from a biosecurity perspective, Thomas added that “they can pivot quickly when the threat changes.”
Most notably, mRNA platform technology enabled the development of the first COVID vaccines from Moderna and BioNTech, the latter in collaboration with Pfizer. Both companies have vaccine candidates for monkeypox. “We are also working on a Nipah vaccine. It's currently in Phase I,” said Sunny Himansu, Associate Director of Infectious Diseases at Moderna.
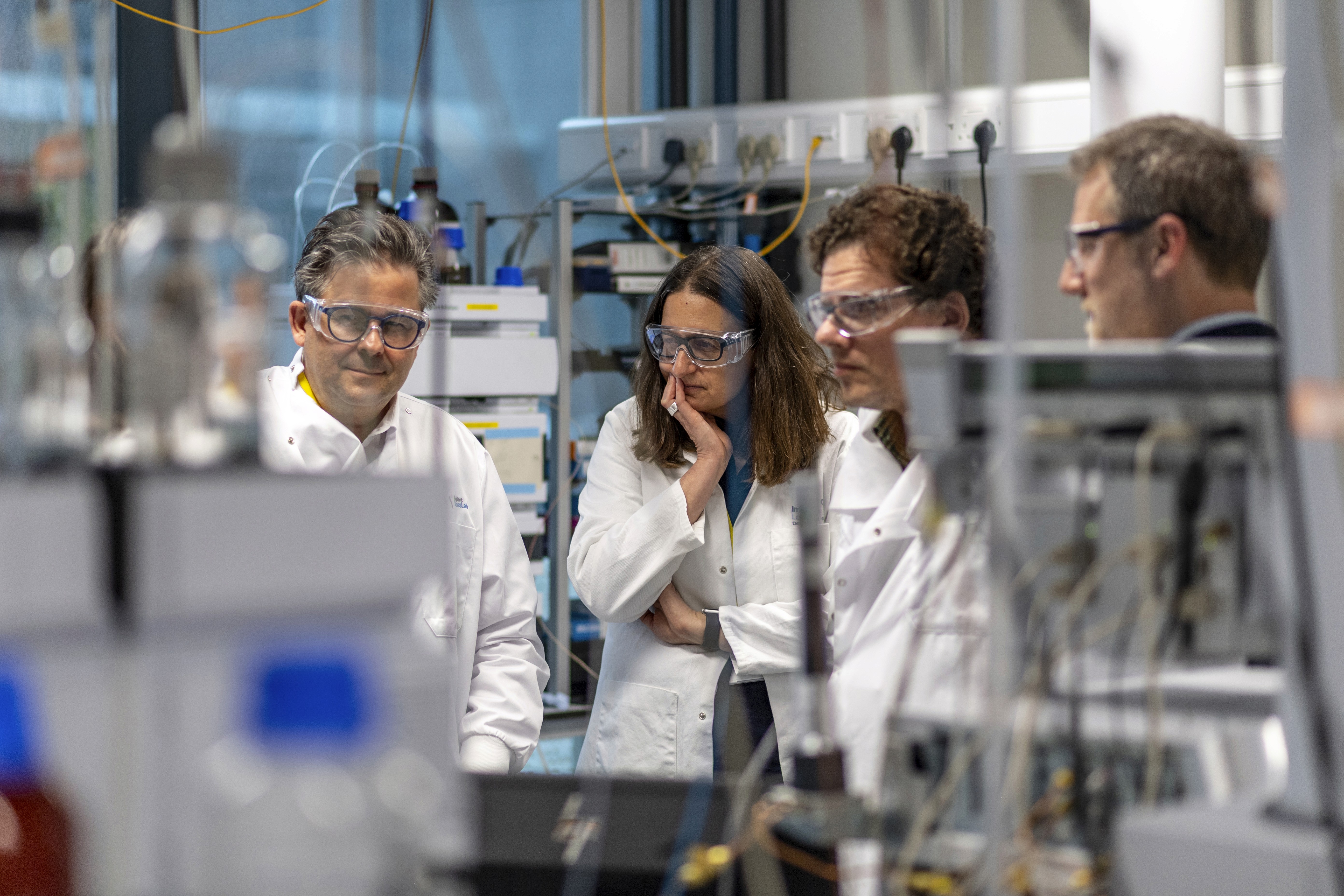
Himansu stressed that every pathogen is different, and each vaccine, even with the same platform, is a unique challenge. Vaccine development benefits from basic research on the biology of the pathogen and vectors. As rare pathogens are often understudied, this slows progress on vaccines and therapeutics against rare infectious diseases.
Even with sufficient background knowledge, if there are few or no cases of a particular rare infection at any time, that makes it near impossible to establish vaccine efficacy, that is to say, what proportion of cases could have been prevented by administering the vaccine.
Many rare infections are endemic to one or a few countries. Himansu said that companies need to work with regulatory bodies to figure out what kind of evidence would work in the absence of vaccine efficacy data. With this approach, French biotech Valneva received accelerated approval from the FDA earlier this month for its chikungunya vaccine. This is the first approved vaccine globally for chikungunya, a rare viral infection transmitted by mosquitoes.
Therapeutics for Rare Infections
While vaccines are generally thought to be preventative, therapeutic vaccines treat diseases by stimulating cellular immunity. While a few therapeutic vaccines have been approved for cancers, there are others in the works that target infectious diseases.
However, not all infections are suited for therapeutic vaccines. “With a lot of infectious diseases, once you're infected, the window for treatment is really small,” said Himansu. The therapeutic vaccine has to act quickly to treat someone before there's a benefit of treatment.”
This is why therapeutic vaccines are more effective against chronic infections. For instance, US biotech Precigen is developing a therapeutic vaccine for recurrent respiratory papillomatosis (RRP), a rare chronic infection caused by the human papillomavirus (HPV). The vaccine generates immune responses to target HPV-infected cells.
Helen Sabzevari, CEO of Precigen, told this author in an email conversation that the vaccine provides a durable immune response and has the ability for repeat dosing. These are vital to mount a sustained attack on an infection. As with Valneva’s vaccine, demonstrating this vaccine’s efficacy will require alternative data.
“FDA has agreed that the ongoing Phase 1/2 single-arm study will serve as pivotal to file an accelerated approval request for licensure,” said Helen Sabzevari, CEO of Precigen. In a single-arm trial, every patient receives the investigational vaccine.
There is a considerable need for non-vaccine therapeutics as well. As fungal infections are most common in immunocompromised patients, devising vaccines against them is challenging. Similarly, vaccines for parasitic infections are problematic as parasites go through multiple life stages during which they might occupy different niches within the host. Further, “immune responses from natural parasitic infections aren't usually durable or life-long,” said Thomas.
Moreover, “they often have thousands of proteins that can serve as targets of vaccines or therapeutics,” said Norbert Pardi, assistant professor of medicine at the University of Pennsylvania. “The correlates of protection are not known—therefore, vaccine/therapeutics development against these pathogens is challenging.”
While a few small molecule drugs exist for rare fungal and parasitic infections, synthetic biology approaches can be more easily generalized to multiple diseases. For instance, phages are emerging as a potent therapeutic approach to bacterial infections. Therapeutic uses of mRNA technology are a subject of active research. “For non-vaccine applications, one key feature is to design the platform to be non-inflammatory or minimize immune activation by the mRNA and/or the delivery molecule,” said Pardi.
Alternatively, synthetic cells combine the benefits of therapeutic vaccines and small-molecule drugs. Synthetic cells can be designed to bind particular DNA or protein sequences, allowing them to attack infected cells with high precision. Due to their customizability and amenability to low-volume manufacturing, they could be a suitable approach to developing on-demand therapeutics for rare infections.
Pandemic Preparedness
Climate change, deforestation, and other anthropogenic stressors are accelerating the rate of zoonotic spillovers. These are events when a pathogen transmits from animals to humans. This raises the threat of new emerging infectious diseases. Developing therapies for rare infections improves preparedness for these potential pandemics.

Before developing therapies, researchers need to be able to detect them quickly. On a global scale, pandemic surveillance approaches, such as monitoring pathogens in wastewater, will enable early identification of new emerging pathogens. Because of the links between climate change and emerging pathogens, pandemic surveillance needs to be climate-conscious. "We need strengthened infectious disease surveillance across both the human and animal sectors, integrated with climate-sensitive forecasting systems in LMICs," Nidhee Jadeja and co-authors wrote in a letter to Nature Microbiology.
At the scale of individual diseases, it is diagnostic tools that matter. Advances in synthetic gene circuits and biosensing technologies now drive the quick development of various diagnostic tests.
In the wake of the COVID pandemic, companies are working on vaccines and therapeutics for prototype pathogens like Nipah. These are pathogens that are representative of pathogen families. They act as excellent benchmarks to test platform technologies and diagnostic modalities.
While Nipah hasn’t blown into a pandemic yet, it could continue mutating in bat reservoirs until a future version is far more deadlier. “If a Nipah-like pathogen comes in the future, we will have enough knowledge to be able to apply and quickly accelerate response to the emerging threat,” concluded Himansu.
The author would like to thank the National Press Foundation for a grant for covering rare diseases. The Foundation did not influence the research or reporting of this article.